Osteochondritis dissecans
What is osteochondritis?
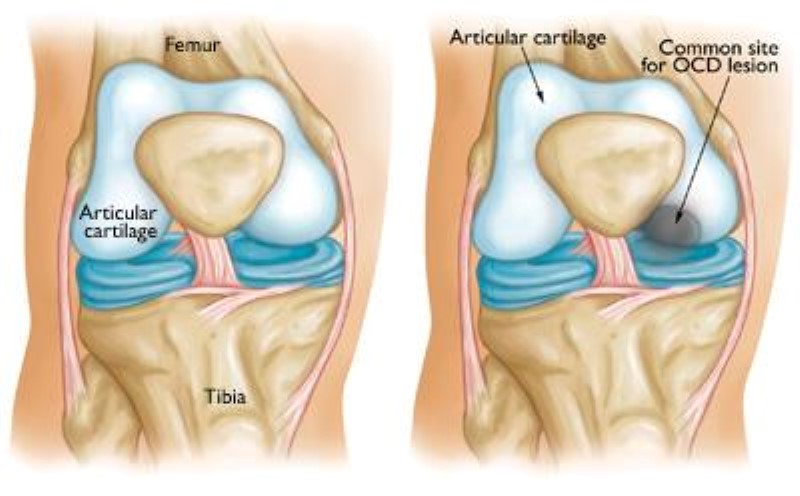
Every bone has an “ossification centre” – a point from which the bone grows. Osteochondritis dissecans (OCD) is a condition that affects these areas making them degenerate (in serious cases, the area of bone may even die) and limiting their capacity to grow normal bone. As a result, pieces of bone and cartilage may come loose or break off. These are called osteochondral loose bodies.
This condition can affect the bones of various joints of the body – knee, elbow, hip or ankle. In the knee, they almost always affect the curved parts at the end of the femur (called femoral condyles), and in particular the medial (or inner) condyle. Very occasionally, the condition may affect the top of the tibia and the patella.
This condition most commonly affects adolescents, and may pass un-noticed, until a loose piece of bone in the joint starts to cause problems. In some cases it may not give any symptoms, and it heals on its own. However, large OC lesions can lead over time to the development of osteoarthritis.
What causes it?
No-one knows for sure what causes OCD: a previous injury, genetic predisposition, and ischemia (a reduction in blood supply) – or a combination of all of these – are possible causes.
How does it feel?
Your knee may ache, and you may hear a clicking noise when you move your leg. Some patients may have a swollen or painful knee, that gets worse with exercise. The knee also may lock if a loose fragment gets caught in the joint.
Diagnosis
Your doctor will ask you about your medical history, and he will make a physical examination of your knee. He may also ask for X-rays and an MRI scan.
Treatment – conservative
As there are various types of lesion, some more serious than others, treatment will depend on the severity of the lesion. Your doctor may prescribe rest, shock wave therapy or magnetotherapy. He may also prescribe anti-inflammatory medication to control the pain and swelling. If it is a large lesion, you may need to walk with crutches for a while. A follow-up and new imaging exams are necessary to ascertain if treatment has been effective and if healing is in progress. Otherwise a surgical option must be considered.
Treatment – surgical
Depending on the size and seriousness of the defect your surgeon may perform one of the following procedures.
Arthroscopic Osteochondral Fragment Stabilisation: if the fragment is firmly attached to the bone, he will drill into it to make the blood flow to this area which promotes healing. If the fragment is loosely attached or even has come away, he will fix it back with absorbable pins or screws.
Osteochondral Graft: the surgeon removes a cylinder of bone tissue which contains the damaged bone and cartilage from the site of the lesion. Then a cylinder of undamaged bone and cartilage, of exactly the same size, is removed from elsewhere in the knee (from a non weight-bearing site). This cylinder is then either glued or press-fitted into the original site of the lesion.
Chondrocyte Transplant (cartilage graft) – during arthroscopy, the surgeon will remove a piece of healthy cartilage, which will then be put in culture. Over the next 4-6 weeks more cartilage cells will grow. These new cells will then be re-injected into the lesion where they should adhere and replicate, creating new cartilage. If the underlying bone is seriously damaged it may be necessary to remove and replace it with a bone graft before injecting the new cells.
Rehabilitation after surgery
You will need to wait 4-8 weeks before being able to walk without crutches. You will start physiotherapy almost immediately to recover your range of movement, and to strengthen your muscles.